CHARM-COPD Project Snapshot
Who: Researchers at the University Health Network (UHN), Sunnybrook Health Sciences Centre, and the University of Toronto (all in Toronto)
What: Remote patient monitoring app for COPD patients, which is designed to capture daily symptom changes and treatment adjustments
Features:
- Digital daily diary for patient symptom tracking
- Real-time patient-clinician chat
- Clinician dashboard with batch review and notifications
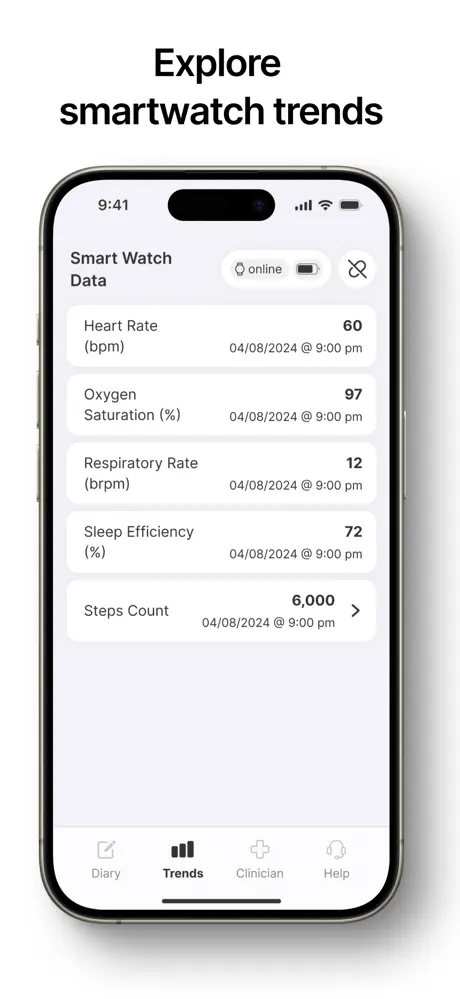
- Fitbit and daily voice recordings for predictive monitoring research purposes
Future Expansion: Developing a programmable platform to adapt to other conditions (hypertension, oncology, inflammatory bowel disease) while maintaining data collection for predictive research
Remote patient monitoring (RPM) has often focused on collecting and analyzing data to detect health events after they occur, such as blood pressure spikes or glucose excursions. But RPM can also be extended beyond detection to prediction. These apps can identify subtle signals that appear before patients themselves notice a change.
In chronic obstructive pulmonary disease (COPD), for example, RPM can mean identifying exacerbations quickly enough to enable clinicians to intervene sooner, to begin treatment, and prevent more serious complications.
This shift is part of a broader transformation in predictive healthcare analytics. A comprehensive literature review published in the National Library of Medicine explored the transformative impact of AI predictive analytics on healthcare. The review emphasized improvements in patient outcomes concerning disease progression, treatment response, and recovery rates, illustrating the potential of AI in enhancing clinical decision-making.
At MindSea, we partnered with the University Health Network (UHN), Sunnybrook Health Sciences Centre, and the University of Toronto to develop and test a COPD remote patient monitoring app. The team designed the Connected, At-Home, Accessible Remote Monitoring in COPD (CHARM-COPD) platform to support daily clinical care and generate the structured datasets needed for predictive research.
Building a Collaborative Blueprint
This project began with a structured UX blueprint phase. We developed the blueprint in collaboration with research teams at UHN, Sunnybrook and the University of Toronto. The goal was to ensure that the app’s functionality aligned with both clinical workflows and research protocols. From the outset, we approached the project with three guiding principles:
- Patient-centered design and usability to improve adherence
- Actionable insights for clinicians
- Reliable data capture for predictive research
We worked closely with researchers and clinicians to define requirements, map workflows, and establish patient use cases. Patient involvement was also central to the design process. We conducted live, face-to-face usability testing with people living with COPD. In the tests, we observed how they interacted with prototypes and refined the interface to remove friction. We also incorporated accessibility standards. Many people living with COPD experience vision limitations, so the app adhered to Web Content Accessibility Guidelines (WCAG) standards, including those related to contrast and font, to ensure clarity and ease of use.
Shifting COPD Care from Reactive to Predictive
According to Dr. Andrea Gershon, Respirologist and Senior Scientist at Sunnybrook Health Sciences Centre, University of Toronto and ICES, insights from research conducted at the University of Ottawa, University College London, and McGill University informed the app’s design, particularly its focus on detecting COPD exacerbations.1 “This then allows treatment to begin as soon as possible and also reduces the risk of hospitalization,” explains Gershon.
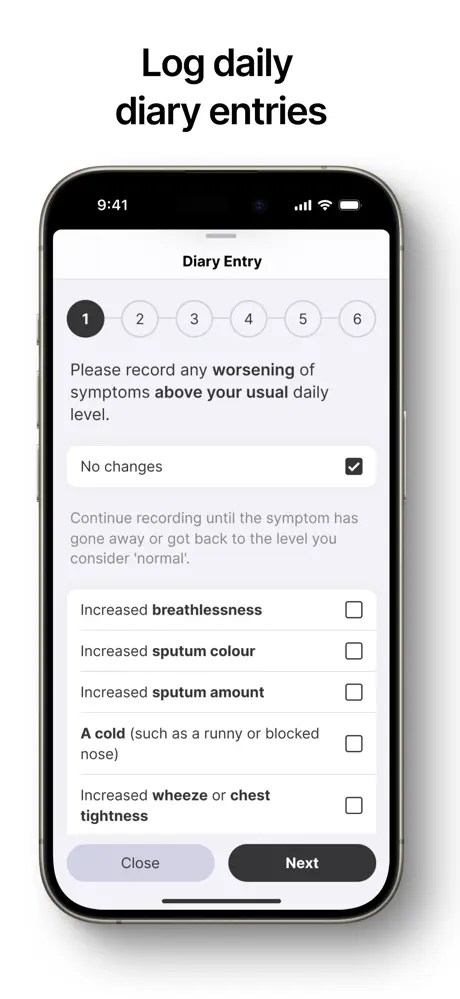
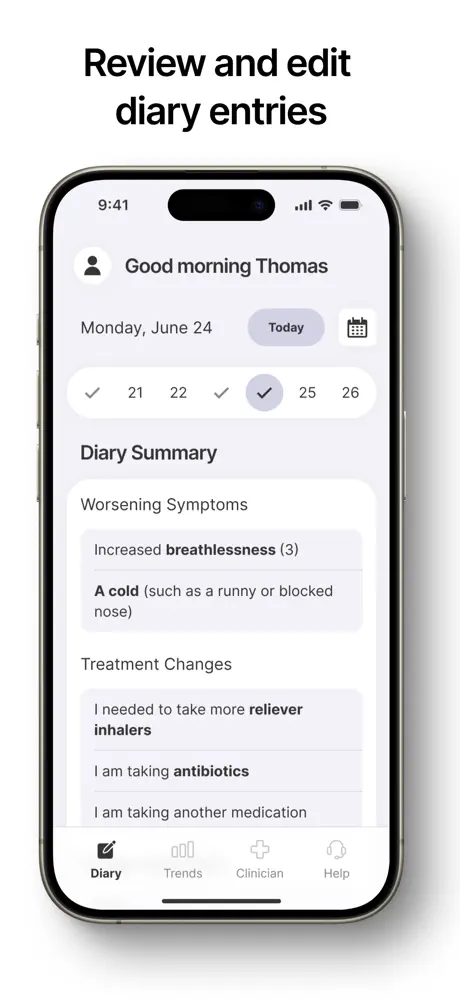
We digitized the COPD daily diary from its traditional paper card format. We then simplified it to capture symptom changes, treatment adjustments, and other relevant health data in a format that patients could easily use.
Patients record daily symptoms and treatment changes, which are then used to calculate a COPD score. When scores exceed pre-defined thresholds for consecutive days, alerts are sent to clinicians so they can intervene promptly, such as adjusting treatments or scheduling visits to prevent hospitalisation.
Alex Mariakakis, Assistant Professor in the Department of Computer Science at the University of Toronto and an Affiliate Scientist at Techna, adds:
“Alongside these measures that are used clinically, CHARM also supports the collection of experimental signals that are helping researchers develop new digital biomarkers. Patients record their voice using a pre-defined sentence, which we can analyze using deep learning to detect subtle changes that precede an exacerbation. We did this in a previous project called PulmoListener2, but CHARM would make it much easier to collect this data in an engaging way along with useful signals from Fitbits and other devices…”
Building Patient Trust and Engagement
Sustained patient engagement is crucial in any remote patient monitoring program, but making sure patients enter their data and record their voice daily can be a challenge. Patients want to understand the benefits of doing this. To overcome this issue and reinforce trust and motivation, the app integrates features that make patient input more meaningful.
Patients can use an online chat with clinicians to discuss symptom changes, clarify treatment adjustments, and gain reassurance that doctors are actively monitoring their symptoms. Knowing that every entry contributes to both their own clinical care and ongoing research motivates patients to maintain daily reporting, strengthening the feedback loop between patient input, clinician response, and predictive insights.
Mariakakis adds: “Patients can also reach out to researchers instead of clinicians if they have technical issues, which removes the burden of IT support from clinicians.”
For doctors, we developed a web-based clinician dashboard to take into account their busy schedules. It provides a clear, at-a-glance overview of all patient data so clinicians can see what matters most in seconds.
The workflow is optimized to minimize clinician burden through the ability to batch review daily diary entries, mark them as seen, and automatically notify patients that their chart has been reviewed. The platform sends email alerts to clinicians when a patient’s condition changes, enabling them to quickly determine whether treatment adjustments or in-person visits are needed to prevent hospitalization. This multi-layered system ensures patients remain engaged, clinicians are kept up to date, and critical interventions can take place promptly.
A key consideration was Electronic Health Record (EHR) integration, as logging into a separate system could be time-consuming and inefficient. To address this, we integrated the CHARM platform with the hospital’s login systems. Clinicians can use their hospital credentials to sign in and access the dashboard automatically with no additional logins required. This not only reduces friction for busy clinicians but also enhances security.
Robert Wu, Clinician Investigator, Toronto General Hospital Research Institute (TGHRI), adds:
“In the future, we will integrate the clinician dashboard directly within the EHR.”
Navigating Organizational and Compliance Challenges
Developing an RPM platform within large hospital networks is complex. This project involved multiple institutions, each with distinct privacy, security, and compliance requirements, plus app store regulations.
MindSea partnered with research teams to navigate these requirements step by step, ensuring the platform met institutional standards without compromising usability or research integrity. This highlighted the fact that implementation challenges in large hospital networks often extend beyond technical development. As a SOC 2–certified organization, MindSea’s focus on security and privacy also reassured partners that these priorities were of paramount importance.
From Single-Condition Tracking to Adaptable Patient Monitoring
In the future, the MindSea team and researchers behind the UHN RPM project will be expanding the functionality to move beyond COPD. We are currently creating a second blueprint to expand this platform to other medical conditions beyond COPD, including hypertension, oncology, and inflammatory bowel disease.
The aim is to make the platform programmable so a researcher can configure and adjust it for any medical condition, rather than including fixed functionality for just one indication. Daily diary questions, for example, would differ depending on the condition. COPD questions will be unique to that population, while hypertension questions will be entirely different.
The purpose of monitoring patients while collecting data to support predictive monitoring would remain the same.
A Model for Future Remote Patient Monitoring Research
This collaboration shows how research-focused remote patient monitoring can not only advance predictive analytics but also deliver real benefits for patients.
Dr. Gershon explains:
“By enabling early detection and proactive intervention, the platform will help reduce hospitalizations, minimize suffering, and provide reassurance in the future. Patients will be able to gain peace of mind knowing their health is closely monitored while their daily quality of life is improved. This demonstrates that carefully designed technology can make healthcare more responsive, supportive, and truly patient-centered.”
RPM Project Blueprint Checklist
For researchers and clinician-researchers considering similar systems, we have developed a checklist that enables you to balance technical development, patient experience, and research goals in RPM projects:
- Start with a blueprint to clarify workflows and objectives before development
- Prioritize patient usability and patient-centered design through iterative testing
- Facilitate meaningful clinician engagement via dashboards and communication tools
- Layer research functionality onto real-world utility to support predictive monitoring depending on the goals of the institution
- Plan for compliance and regulatory hurdles early, particularly across multiple institutions
Footnotes
1 Aaron SD, Donaldson GC, Whitmore GA, Hurst JR, Ramsay T, Wedzicha JA. Time course and pattern of COPD exacerbation onset. Thorax. 2012;67(3):238–243. doi:10.1136/thoraxjnl-2011-200768
2 Bhalla S, Liaqat S, Wu R, Gershon AS, de Lara E, Mariakakis A. Pulmolistener: Continuous Acoustic Monitoring of Chronic Obstructive Pulmonary Disease in the Wild. Proceedings of the ACM on Interactive, Mobile, Wearable and Ubiquitous Technologies. 2023 Sep 27;7(3):1-24. doi:10.1145/3610889